Česká a slovenská psychiatrie

Časopis
Psychiatrické společnosti ČLS JEP
a Psychiatrickej spoločnosti SLS
původní práce / original article
REPORTOVANÉ ZDRAVOTNÉ PROBLÉMY U PACIENTOV S REUMATOIDNOU ARTRITÍDOU A ICH PREFERENCIE PRE NEFARMAKOLOGICKÉ INTERVENCIE
SELF-REPORTED HEALTH PROBLEMS AND PATIENTS´ PREFERENCES FOR NON-PHARMACOLOGICAL INTERVENTIONS IN RHEUMATOID ARTHRITIS
Alexandra Husivargova1,2, Esther Sulkers2, Zelmíra Macejova3, Zuzana Kotradyova3, Dagmar Breznoscakova 1, Robbert Sanderman2,4, Joke Fleer2, Iveta Nagyova1
1 Department of Social and Behavioural Medicine, Faculty of Medicine, PJ Safarik University in Kosice, Slovak Republic
2 Department of Health Psychology, University Medical Center Groningen, University of Groningen, The Netherlands 3 1 st Department of Internal Medicine, Faculty of Medicine, PJ Safarik University in Kosice, Slovak Republic
4 Department of Psychology Health and Technology, University of Twente, The Netherlands
2 Department of Health Psychology, University Medical Center Groningen, University of Groningen, The Netherlands 3 1 st Department of Internal Medicine, Faculty of Medicine, PJ Safarik University in Kosice, Slovak Republic
4 Department of Psychology Health and Technology, University of Twente, The Netherlands
This work was supported by the Slovak Research and Development Agency under contract APVV-15-0719.
Táto práca bola podporovaná Agentúrou na podporu výskumu a vývoja na základe Zmluvy č. APVV-15-0719.
SÚHRN
Husivargova A, Sulkers E, Macejova Z, Kotradyova Z, Breznoscakova D, Sanderman R, Fleer J, Nagyova I. Reportované zdravotné problémy u pacientov s reumatoidnou artritídou a ich preferencie pre nefarmakologické intervencie
Cieľ: Výskumy poukazujú na potencionálny pozitívny vplyv nefarmakologických intervencií (NPI), ako je fyzioterapia a kognitívno-behaviorálna terapia (CBT) , na zdravotné výsledky u pacientov s chronickým ochorením. Aby sa uľahčila implementácia NPI založených na dôkazoch, prvým krokom je porozumieť širšiemu zdravotnému kontextu pacientov a ich preferencií ohľadom manažovania ochorenia. Cieľom tejto štúdie bolo preskúmať seba-reportované zdravotné problémy (SRHP) a záujem o NPI u pacientov s reumatoidnou artritídou (RA) podstupujúcich biologickú liečbu.
Materiál a metódy: Výskumný súbor pozostával z 183 pacientov s RA (80,9 % žien; priemerný vek 55,6 ? 13,5 roka) z reumatologickej ambulancie v Košiciach na Slovensku. Otvorené otázky o SRHP a preferencie pre NPI, spolu so sociodemografickými (vek, pohlavie, vzdelanie, zamestnanie a bydlisko) a environmentálnymi charakteristikami (internetové pripojenie v domácnosti, vzdialenosť bydliska od nemocnice a doprovod do nemocnice) boli zozbierané prostredníctvom telefonického rozhovoru. Klinické charakteristiky pacientov (HAQ-DI, DAS28, dĺžka ochorenia a biologickej liečby) boli získané zo zdravotných záznamov.
Výsledky: Fyzické zdravotné problémy uvádzalo 63,9 % pacientov a kombinované fyzické a mentálne problémy uvádzalo ďalších 33,3 %. Pacienti s viacerými SRHP (χ2 = 9,091, p < 0,01) a používatelia internetu (x2 = 14,380, p < 0,001) mali väčšiu pravdepodobnosť záujmu o NPI. Nenašli sme žiadne významné asociácie medzi preferenciou pre určitý typ NPI a sociodemografickými, klinickými, či environmentálnymi charakteristikami.
Záver: Prevažná väčšina pacientov s RA bola otvorená NPI ako novému druhu doplnkovej liečby. Naše výsledky by mohli byť prínosom pre klinickú prax, nakoľko môžu napomôcť pri prispôsobovaní intervencií na základe najdôležitejších SRHP pacientov.
Klíčová slova: kognitívno-behaviorálna terapia, nefarmakologické intervencie, fyzioterapia, reumatoidná artritída, seba-reportované zdravotné problémy
SUMMARY
Husivargova A, Sulkers E, Macejova Z, Kotradyova Z, Breznoscakova D, Sanderman R, Fleer J, Nagyova I. Self-reported health problems and patients´ preferences for non-pharmacological interventions in rheumatoid arthritis
Objective: There is promising evidence for the positive impact of non-pharmacological interventions (NPIs) such as physiotherapy and cognitive behavioural therapy (CBT) in patients with a chronic disease. To facilitate the implementation of evidence-based NPIs, a first step is to understand patients´ self-reported health problems (SRHPs) and their preferences for NPIs. This study aimed to explore patients´ SRHPs and interests in NPIs in patients with rheumatoid arthritis (RA) undergoing biological treatment.
Methods: We included 183 RA patients (80.9% females; mean age 55.6 ? 13.5 years) from the rheumatology outpatient department in Kosice, Slovakia. Open questions about SRHP and NPI preference, along with sociodemographic (age, gender, education, employment status, area where patient live) and environmental characteristics (home internet connection, distance from home to hospital, and companion on hospital visits) were collected through a telephone interview. Clinical characteristics of patients (HAQ-DI, DAS28, duration of disease and biologic therapy) were obtained from their medical records.
Results: Physical health problems were reported by 63.9% of patients, and combined physical and mental health problems by an additional 33.3%. Patients with multiple SRHPs (χ2 = 9.091, p < 0.01) and Internet users (x2 = 14.380, p < 0.001) were more likely to be interested in NPIs. We found no significant associations between a preference for a certain type of NPI and sociodemographic, clinical, or environmental characteristics.
Conclusions: The majority of RA patients were open to NPIs as a new kind of additional treatment. Our results could benefit practice by helping to tailor interventions based on the patients´ most important SRHPs.
Key words: cognitive behavioural therapy, non-pharmacological interventions, physiotherapy, rheumatoid arthritis, self-reported health problems
INTRODUCTION
Rheumatoid arthritis (RA) is regarded as one of the most common chronic autoimmune diseases in the world with a prevalence of 0.4-1.3%.1,2 Onset most often occurs during middle age and females are affected three-times more often than males.1,3,4 The main cause of RA is unknown, but it is understood that genetics, environmental, and several other factors, such as behavioural factors and sociodemographics (sex, age or working conditions), are responsible for the cause of the disease.3,4
A diagnosis of RA entails multiple health problems which have implications for an individual in physical, psychological, and socioeconomic areas of life. 1, 5-9 The main physical complaints reported by RA patients are pain, disability, and fatigue.5,10-12 The prevalence of fatigue varies between 42-80% for clinically relevant fatigue and 40% for persistent severe fatigue.4,11,12 In addition to physical health problems, many patients suffer from mental health problems, including depression and anxiety,1,2,5,13-15 and fear and worry about their future.7 Physical and mental health problems mutually influence each other and can lead to further deterioration of the disease and reduced quality of life.1,12,15-17
RA is a chronic disease that cannot be cured, but medication is used to control it. Biological treatment is one of the newest types of RA treatments used in patients unresponsive to synthetic Disease-Modifying Anti-Rheumatic Drugs (sDMARDs).2,3,10 Additional to pharmacological treatment, non-pharmacological interventions (NPIs) are available for the management of RA, such as psychological and physical therapies. There is evidence suggesting that increasing physical activity and/or exercise can simultaneously improve symptoms and reduce the impact of systemic manifestations in RA.6,17 Another beneficial NPI is Cognitive Behavioural Therapy (CBT), which is a widely used form of psychotherapy aimed at identifying and changing maladaptive patterns of thought and behaviour.9,16 Both types of interventions have been proven to be effective in reducing fatigue, pain, disability, depression, and helplessness and improving sleep and quality of life in RA.2,10,12,17 One of the newer intervention options is online CBT. Using CBT through eHealth (computer, tablet or mobile phone) may help patients overcome some of the limitations, such as travelling long distances, and patients appreciate its comfort and flexibility.18,19 Online CBT intervention programs have demonstrated similar efficacy as in-person CBT.20 With regard to specific characteristics, younger RA patients use the Internet more often and they are more open to online eHealth programs than older RA patients. Similarly, females tend to seek psychological help (live or via eHealth) more often than males.21,22
NPIs for RA are rather frequently used in Western Europe, but relatively rarely in Central and Eastern European (CEE) countries, including in the Visegrad four Group countries (Czech Republic, Hungary, Poland, and Slovakia).23 The focus of RA treatment in these latter countries is mostly pharmacological; and physicians in their everyday practice prioritize biomedical approaches as opposed to the bio-psycho-social model.17
To facilitate the implementation of evidence-based NPIs, a first step is to understand patients´ self-reported health problems (SRHPs) and their preferences for NPIs. This is important within the context of patient-centered care and shared decision making, as recent studies indicate that patient involvement in medical decisions may lead to improved outcomes and better adjustment.9,18,24
As such, this study aims to answer the following research questions:
1. What are the most frequent RA-related SRHPs of RA patients?
2. Are RA patients interested in NPIs? If so; what type of NPIs do they prefer?
3. Which sociodemographic, clinical, and environmental characteristics are associated with patients´ preferences for NPIs (a) in general and (b) for a certain type of intervention, such as CBT (live or online), or physiotherapy?
METHODS
Sample and procedure
The study sample was recruited from the rheumatology outpatient department in Kosice, eastern Slovakia, which specializes in biological treatment. Inclusion criteria for participating in the study was to be diagnosed with RA, based on the criteria of the American College of Rheumatology published in 1987,25 and age younger than 18 years at study entry. Patients who were unable to understand the Slovak language were excluded from the study. Data collection via telephone interview took place between April and June 2018 (9 weeks in total). Clinical characteristics were retrieved from medical records. The time difference between data acquired within the telephone interview and clinical data was maximum of 14 days.
Out of 205 individuals who were found eligible, 9 patients (4.4%) did not answer the telephone and 13 (6.4%) did not have a valid telephone number in the rheumatologist?s database. Every patient was called several times. Patients not available at the moment were contacted again (at minimum 10x) at various times of the day. The final sample consisted of 183 patients (response rate of 89.3%). The study was approved by the Ethics committee of the Faculty of Medicine, PJ Safarik University in Kosice under number 115/2011 and patients signed informed consent.
Measures
Sociodemographic and environmental characteristics
Sociodemographic characteristics, such as age, gender, and a patient´s address, were retrieved from the medical records. Based on the address, patients were grouped into urban/rural areas and the distance (in km) from the hospital was computed. Information on education, employment status, companion on a hospital visit, and internet use were gathered via the telephone interview.
Clinical characteristics
Clinical characteristics on disease severity and disease activity, which are collected within a routine medical examination, were retrieved from medical records. Disease activity was assessed via the Erythrocyte Sedimentation Rate (ESR) during the first hour (mm/1st hour). Tender and the swollen joint count were also examined. Patients assessed their disease activity on a visual analogue scale, and a comprehensive Disease Activity Score (DAS28) was calculated for each patient.26
Functional disability was measured using the Health Assessment Questionnaire-Disability Index (HAQ-DI). The HAQ-DI includes items that assess fine movements of the upper extremities and locomotor activities of the lower extremities, both related to ability to carry out activities of daily living.27 A higher score represents greater functional disability. The Slovak version of the HAQ-DI has adequate reliability and construct validity.28 Cronbach´s alpha in our sample yielded 0.86.
Self-reported health problems related to RA
Patients were asked with an open question if they could identify the most frequent SRHPs related to having RA. The interviewer registered all the health problems that patients reported. The SRHPs were categorized into physical problems (such as pain, fatigue, functional disability, and morning stiffness) and psychological problems (such as feeling sad, feeling depressed, and feeling lonely).
Interest in non-pharmacological interventions
Patients received a short explanation regarding types of NPIs which were about to become available at the rheumatology outpatient clinic (i.e. physiotherapy, CBT, and online CBT). Subsequently, they were asked whether they were interested in NPIs in general and which type(s) of intervention they would consider helpful in particular.
Statistical analyses
Descriptive statistics (means, standard deviations, range, and percentages) were used to describe the characteristics of the sample. The associations between the interest in NPIs and the explanatory variables were analysed in bivariate analyses using Chi-Square tests and t-tests. A p-value of 0.05 was considered statistically significant. The analyses were performed using the Statistical Package for the Social Sciences (SPSS 23; IBM). Post-hoc power analysis revealed that the statistical power for bivariate analysis with 183 patients exceeds 96%, with a medium effect size at α = 0.05.29
RESULTS
Sample characteristics
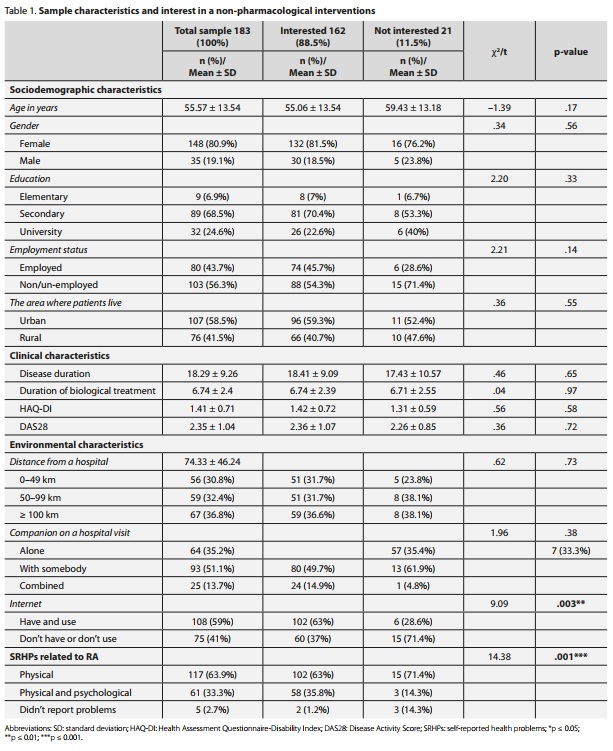
The majority of the RA patients were females and middleaged, with mean age 55.6 ? 13.5 years. The mean disease duration was 18.3 ? 9.3 years. Patients´ disease activity was low DAS28 and functional disability (HAQ-DI) was moderate to severe (tab. 1). More than half of patients were non/un-employed. Most of the patients lived in urban areas and relatively far from a hospital (mean 74.3 km, ranging from 0-198 km). The rate of access to the Internet was high (87%); however, only a little bit more than half of the patients were actually using it (tab. 1).
Self-repported health problems and preference for non-pharmacological interventions
With regard to SRHPs, the majority of the patients reported only physical problems. Pain, fatigue, functional disability, and morning stiffness were mentioned most often. One-third of the patients reported both physical and psychological problems. The most common psychological problems were feeling sad, feeling depressed, and feeling lonely. Nearly three percent of the RA patients reported having no problems at all.
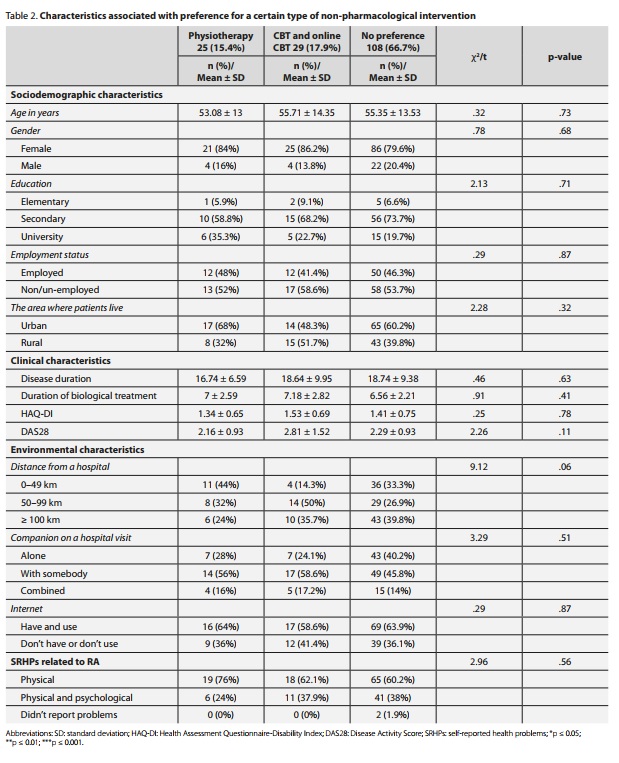
As to NPIs, the results show that majority of the RA patients were interested in some type of NPIs to improve their daily life (tab. 1). Of the 162 patients who expressed interest in NPI, 108 patients had no specific preference for a certain type of NPI. Of the patients who were interested in a certain type of intervention, 25 were interested in physiotherapy, and 29 in CBT (of which 18 patients preferred in-person CBT and another 10 RA patients preferred especially online CBT as a suitable NPI) (tab. 2).
Sociodemographic, clinical, and environmental characteristics associated with the preference for NPIs, in general and for a certain type of intervention
Patients with multiple SRHPs had a stronger preference for NPIs as compared to patients reporting fewer SRHPs (χ2 = 14.4, p < 0.001). Similarly, patients who have and use the Internet were also more interested in NPIs = 9.1, p < 0.003) when compared to patients who did not have or did not use the Internet. None of the other characteristics were significantly associated with preference for NPI in general (tab. 1).
The preference for a certain type of NPI (physiotherapy, CBT, online CBT) was not associated with any of the sociodemographic, clinical or environmental characteristics. Also, there was no significant association found between the preference for a certain type of NPI and the type of SRHPs (i.e. physical or both physical and psychological). Although non-significant, the analyses revealed a tendency to prefer a certain type of intervention based on the physical distance. Patients who lived closer to the hospital preferred physiotherapy, whereas patients who lived farther from the hospital preferred CBT (face-to-face or online CBT) (tab. 2).
DISCUSSION
This study aimed to explore RA patients´ self-reported health problems (SRHPs) and preferences for non-pharmacological interventions (NPIs). The results show that despite biological treatment, patients still encounter a relatively high number of physical problems and to a lesser extent also psychological problems. Moreover, the results reveal that the majority of RA patients would welcome a certain type of NPI in addition to their standard treatment, and that patients´ interest in NPI was statistically significantly associated with Internet availability and its usage as well as with a total number of SRHPs.
Our results are in line with earlier studies indicating that RA patients experience many problems in their lives. The majority of patients report high levels of physical health problems, such as pain, functional limitations, and fatigue.1,2,10,11 Psychological problems, including feelings of being depressed, sad or lonely, were also mentioned by our patients, but to a much lesser extent and never independently from physical problems. The prevalence of depression in earlier studies on RA ranged broadly, from 0.04% and 66.3%, and anxiety between 13% and 70%.14,15 In our study, feeling depressed or sad was mentioned by approximately 26% of patients, whereas feeling anxious was not mentioned at all. There are several explanations for our findings. Firstly, the telephone interviews were carried out by research staff from the rheumatology outpatient department, so patients may have focused more on physical problems rather than a broader range of problems, including psychological symptomatology. Secondly, the discrepancies between our findings and those of other studies could be also due to the different methodologies used, i.e. the open question format used in our study vs. the use of standardized questionnaires in other RA studies in which patients were specifically asked about mental health, depression, anxiety, etc.5 Thirdly, the findings could be due to cultural differences. Slovak citizens might have negative social responses (e.g. prejudice and unfavourable behaviour) towards mental illness and psychiatric patients30, 31 compared to Western countries where people are more open to visiting a psychologist or psychiatrist.32 This may consequently lead to denial of anxiety and depression in RA patients and to an unwillingness to seek help.33,34
Lastly, in contrast to earlier studies, the participants in this study received biological treatment. Thus, it may be assumed that this specific group of RA patients undergoing biological treatment feels much better compared to RA patients on conventional pharmacological treatment.11
In this study, we also explored patients´ interests in NPIs and we found that the majority of patients in this study were interested in some form of NPI, in addition to biological treatment, which may be beneficial in the management of RA. The findings support previous evidence that physical activity and psychological interventions have the potential to reduce patients´ SRHPs. 2,6,9,10,12,16,20 The majority of patients, but especially those reporting more problems, were interested in some type of NPI in addition to biological treatment, which is a positive finding for the possible more frequent use of the NPIs2. We also found that patients who have and use the Internet were significantly more interested in NPIs than those without the ability to use the Internet. This may be because those RA patients who use the Internet in our study were significantly younger, employed, and living in an urban setting.21,22
Patients who expressed interest in NPIs mostly had no specific preference for either physiotherapy or psychological intervention (CBT). The positive attitude towards CBT (in-person or online) is surprising bearing in mind that most of the SRHPs mentioned were physical and that Slovak patients are inclined to have a somewhat reluctant attitude towards professional psychiatric or psychological support.35 The fact that some patients were interested in online CBT is interesting. Over time, when online eHealth interventions become more common, online CBT might be a promising intervention and a good alternative to inperson CBT.18,20 Even though only a small percentage of patients expressed a specific interest in online CBT, more than half of the patients in this study had and used the Internet and the percentage of people connected to it is increasing. This can be beneficial especially for RA patients as it can overcome problems with travelling due to physical problems; and it can also save money and travelling time.18,19 Also, online therapies are especially useful in a time of COVID-19 or other pandemics, because chronic patients are at higher risk of severe complications.
Lastly, we explored whether patient-related characteristics could be linked with a preference for a certain type of NPI, but we found no significant associations between intervention preference and sociodemographic, clinical, or environmental characteristics. There was also no significant association found between the type of SRHPs and the preference for a certain type of intervention. Although we did not found any significance in preference for a certain type of intervention, the results have shown that nearly three-quarters of our patients were interested in NPIs. This may indicate that current healthcare system is not adequately designed to deal with patients´ symptoms and problems. In previous studies in RA patients, the unmet healthcare needs were related to the consequences of the disease, such as fatigue, pain, impaired function, and psychosocial problems. The most frequently reported complaints in these studies were poor access to a variety of health care services and interventions, lack of time with the rheumatologists, absent multidisciplinary team care, lack of respect, communication, and lack of holistic care.4,9,18,24 Our results can provide additional insights into further improvements of the quality of health care so that it is more responsive to the patients´ needs.
STRENGTHS AND LIMITATIONS
To our knowledge, this is the first study via a telephone interview with open questions examining the associations between SRHPs and interest in NPIs in RA patients undergoing biological treatment. Furthermore, the sample size of this study (with a high response rate) was relatively large. Another strength is that the patients in our sample were asked open questions rather than having to complete a standardized questionnaire. In this way patients could describe their SRHPs and speak about them without the limitation of a structured answer format. On the other hand, we can also consider this as a limitation, as the lack of standardized questionnaires makes it hard to compare with other studies. Another study limitation was that the data were collected from one rheumatology clinic and that all patients were from the eastern part of Slovakia. This might influence the generalization of the results, but considering the relatively small differences in sociodemographics or healthcare between Slovakian regions, this is unlikely.
CONCLUSIONS
The results of this study indicate that the majority of RA patients are open to NPIs as a new kind of additional treatment. This is promising given the fact that there is ample evidence for the positive impact of NPIs such as physiotherapy and CBT in patients with a chronic disease.
Our results could benefit practice by helping us tailor interventions based on the patients´ most important SRHPs, such as pain, functional disability, and fatigue.
AUTHORS´ NOTE
We confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story. Any underlying research materials related to this article can be accessed on demand.
ACKNOWLEDGEMENTS
The authors would like to thank the patients with rheumatoid arthritis who participated in this study. This work was supported by the Slovak Research and Development Agency under contract APVV-15-0719.
DECLARATION OF CONFLICTING INTERESTS
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
REFERENCES
- 1. Espinoza G, Maldonado G, Narvaez J et al. Beyond Rheumatoid Arthritis Evaluation: What are We Missing?. Open Access Rheumatology: Research and Reviews 2021; 13: 45-55.
- 2. Santos EJ, Duarte C, Marques A et al. Effectiveness of non-pharmacological and non-surgical interventions for rheumatoid arthritis: an umbrella review. JBI Evidence Synthesis 2019; 17 (7): 1494-1531.
- 3. Aletaha D, Smolen JS. Diagnosis and Management of Rheumatoid Arthritis. JAMA 2018; 320 (13): 1360.
- 4. Crotti C, Biggioggero M, Becciolini A, Favalli EG. Sarilumab: patient-reported outcomes in rheumatoid arthritis. Patient Related Outcome Measures 2018; 9: 275-284.
- 5. Hitchon CA, Zhang L, Peschken CA et al. The validity and reliability of screening measures for depression and anxiety disorders in rheumatoid arthritis. Arthritis Care & Research 2019; 72 (8): 1130-1139.
- 6. Metsios GS, Kitas GD. Physical activity, exercise and rheumatoid arthritis: effectiveness, mechanisms and implementation. Best Practice & Research Clinical Rheumatology 2018; 32 (5): 669-682.
- 7. Park JY, Howren AM, Davidson E, De Vera MA. Insights on mental health when living with rheumatoid arthritis: a descriptive qualitative study of threads on the Reddit website. BMC Rheumatology 2020; 4 (1): 1-9.
- 8. Shinan-Altman S, Afuta-Goldstein S. Contribution of the self-regulation model to understanding the health related quality of life of rheumatoid arthritis patients. Quality of Life Research 2019; 29 (2): 403-412.
- 9. Sturgeon JA, Finan PH, Zautra AJ. Affective disturbance in rheumatoid arthritis: psychological and disease-related pathways. Nature Reviews Rheumatology 2016; 12 (9): 532542.
- 10. Carpenter L, Barnett R, Mahendran P et al. Secular changes in functional disability, pain, fatigue and mental well-being in early rheumatoid arthritis. A longitudinal meta-analysis. Seminars in Arthritis and Rheumatism 2020; 50 (2) : 209-219.
- 11. Choy EH. Effect of biologics and targeted synthetic disease-modifying anti-rheumatic drugs on fatigue in rheumatoid arthritis. Rheumatology 2019; 58 (5): 51-55.
- 12. Katz P. Causes and consequences of fatigue in rheumatoid arthritis. Current Opinion in Rheumatology 2017; 29 (3): 269-276.
- 13. Berner C, Erlacher L, Fenzl KH, Dorner TE. A cross-sectional study on self-reported physical and mental health-related quality of life in rheumatoid arthritis and the role of illness perception. Health and Quality of Life Outcomes 2018; 16 (1): 238.
- 14. Li N, Chan E, Peterson S. The economic burden of depression among adults with rheumatoid arthritis in the United States. Journal of Medical Economics 2019; 22 (4): 372-378.
- 15. Marrie RA, Hitchon CA, Walld R et al. Increased burden of psychiatric disorders in rheumatoid arthritis. Arthritis Care & Research 2018; 70 (7): 970978.
- 16. Shen B, Li Y, Du X et al. Effects of cognitive behavioral therapy for patients with rheumatoid arthritis: a systematic review and meta-analysis. Psychology, Health & Medicine 2020; 25 (10): 1-13.
- 17. Tali M. A biopsychosocial perspective on health-related quality of life in rheumatoid arthritis. Alkalmazott Pszichologia 2014; 14 (4): 133-148.
- 18. Chehade MJ, Yadav L, Kopansky-Giles D et al. Innovations to improve access to musculoskeletal care. Best Practice & Research Clinical Rheumatology 2020; 34 (5): 101559.
- 19. Wright JH, McCray LW, Eells TD, Gopalraj R, Bishop LB. Computer-Assisted Cognitive-Behavior Therapy in Medical Care Settings. Current Psychiatry Reports 2018; 20 (10): 92.
- 20. Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlof E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cognitive Behaviour Therapy 2017; 47 (1): 1-18.
- 21. Liddon L, Kingerlee R, Barry JA. Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. British Journal of Clinical Psychology 2017; 57 (1): 42-58.
- 22. Wallin E, Maathz P, Parling T, Hursti T. Self-stigma and the intention to seek psychological help online compared to face-to-face. Journal of Clinical Psychology 2018; 74 (7): 1207-1218.
- 23. Dissanayake RK, Bertouch JV. Psychosocial interventions as adjunct therapy for patients with rheumatoid arthritis: a systematic review. International Journal of Rheumatic Diseases 2010; 13 (4): 324-334.
- 24. Hibbard JH, Greene J. What The Evidence Shows About Patient Activation: Better Health Outcomes And Care Experiences; Fewer Data On Costs. Health Affairs 2013; 32 (2): 207-214.
- 25. Arnett FC, Edworthy SM, Bloch DA et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 1988; 31 (3): 315-324.
- 26. Fransen J, Stucki G, van Riel PLCM. Rheumatoid arthritis measures: Disease Activity Score (DAS), Disease Activity Score-28 (DAS28), Rapid Assessment of Disease Activity in Rheumatology (RADAR), and Rheumatoid Arthritis Disease Activity Index (RADAI). Arthritis & Rheumatism 2003; 49 (5): 214-224.
- 27. Bruce B, Fries JF. The health assessment questionnaire (HAQ). Clinical and experimental rheumatology 2005; 23 (5): 14-18.
- 28. Szilasiova A, Macejova Z, Nagyova I et al. Reliabity and Validity of the Slovak Version and Modification of the Stanford Health Assessment Questionnaire-Functional Disability Index (HAQ) in Patient with Rheumatoid Arthritis (RA). Vnitrni lekarstvi 2002; 48 (1): 8-16.
- 29. Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods 2009; 41 (4): 1149-1160.
- 30. Janoušková M, Formánek T, Bražinová A et al. Attitudes towards People with Mental Illness and Low Interest in Psychiatry among Medical Students in Central and Eastern Europe. Psychiatric Quarterly 2020; 92 (1): 407-418.
- 31. Škodová Z, Polčová I. Stigmatization and attitudes towards mental health disorders among adolescent in Slovakia. Kontakt 2020; 22 (1): 54-59.
- 32. Beldie A, Brain C, Figueira ML et al. Stigma in Midsize European Countries. In: Gaebel W, Rossler W, Sartorius N (eds). The Stigma of Mental Illness - End of the Story?. Springer, Cham 2017; 417432.
- 33. Brazinova A, Hasto J, Levav I, Pathare S. Mental Health Care Gap: The Case of the Slovak Republic. Administration and Policy in Mental Health and Mental Health Services Research 2019; 46 (6): 753-759.
- 34. Heretik A, Mullerová Z. Depresia očami občanov Slovenskej republiky. Sociálne reprezentácie pojmu depresia u prispievatelov v on-line diskusii v článku o výsledkoch EPID štúdie v denníku SME. [Depression by citizens of Slovak Republic. Social presentation of depression by on-line participants discussing an article on the EPID study results in daily SME]. Psychiatria 2005; 12 (1): 15-27.
- 35. Soósová MS, Macejová Ž, Zamboriová M, Dimunová L. Anxiety and depression in Slovak patients with rheumatoid arthritis. Journal of Mental Health 2016: 26 (1): 21-27.